Abstract
Introduction The pathophysiology of sickle cell disease (SCD) is complex and goes beyond red blood cell (RBC) sickling alone. Neutrophils have been proposed to play an important role in SCD pathophysiology, but their exact contribution remains to be elucidated. Factors such as chronic hemolysis and oxidative stress can influence neutrophil adhesion, activity and aging. We designed a prospective study (Notice) to investigate a broad set of neutrophil characteristics in SCD patients. To correlate treatment effects of hydroxyurea (HU) on neutrophils with those on RBCs in SCD, we also studied RBC sickling and adhesion. Here, we will focus on the effects of hydroxyurea on RBC deformability and neutrophil adhesion, activity and aging.
Aim: To assess the effects of HU on RBC deformability and neutrophil phenotypes with respect to adhesion, activation and aging.
Methods Blood (EDTA) was collected from SCD patients with HbSS or HbSβ0 in steady-state. A subgroup of patients was included before and during treatment with HU.
For measurement of antigen expression by flow cytometry, total leukocyte fraction after lysis of red blood cells (without Percoll gradient) was used and neutrophils were gated based on their forward and side scatter. For in vitro neutrophil adhesion, neutrophils were isolated using a Percoll gradient and lysis buffer, as previously described. (Kuijpers et al. Blood 2007) Neutrophils were labeled with calcein and placed in an uncoated 96-well MaxiSorp plate. After washing, adherent cells were lysed and fluorescence was measured. (Kuijpers et al. J Allergy Clin Immunol 2017). Adhesion of RBCs was measured by flowing whole blood (20x106/ml)over laminin-coated Ibidi slides for 30 minutes with visualization by microscope. Percentage of mean RBC adhesion was normalized to a healthy control (HC). Data were analyzed using SPSS and GraphPad Prism and are presented as mean ±SE or ±SD as appropriate. Conventional statistics were used.
Results A total of 49 patients (median age 25.0 (IQR 20.0 - 32.5) years, 39% female) were included. Twenty patients (41%) used a stable dose of HU at baseline. In 10 patients, blood was drawn before and after starting HU treatment.
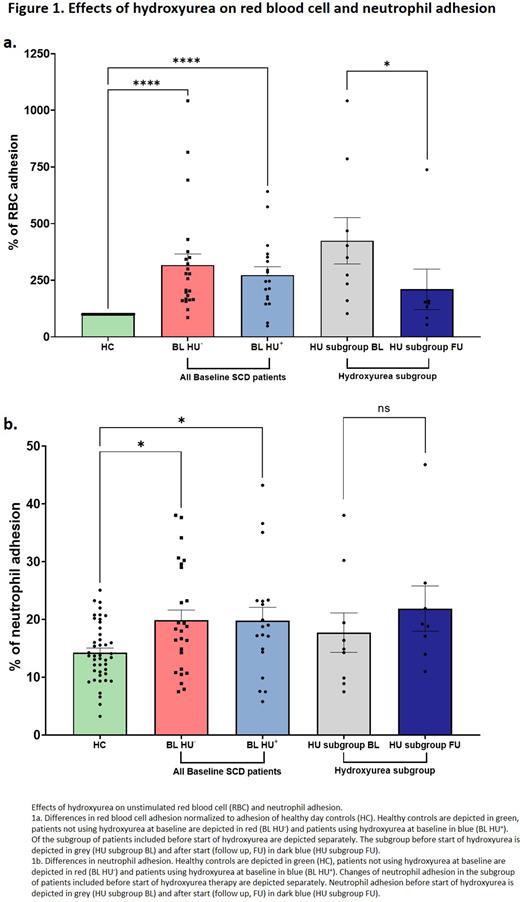
HU treatment improved hemoglobin F and markers of hemolysis and was associated with a decrease in the point of sickling (PoS) of RBCs (from median 24.8 mmHg [IQR 16.0-28.2] to 16.8 [15.0-20.8], P=0.13). Adhesion of RBC was more than 3-fold higher in SCD patients than in HC. At baseline, there was no difference in RBC adhesion between patients with and without HU (P=0.86). After starting HU treatment, RBC adhesion decreased significantly from a median of 318% (normalized to control) to 149% (P=0.016, Figure 1a-b).
Adhesion of neutrophils was significantly higher in patients compared to HC (median 18.3% versus 12.6% P <0.0001). No difference was observed between patients with and without HU at baseline. Neutrophil adhesion did not decrease after starting HU treatment (Figure 1c-d). Neutrophil surface expression of CD11b/CD18 was measured as markers of adhesion. While CD11b expression was comparable between SCD patients and HC, CD18 expression was significantly higher in SCD patients (mean MFI 12193 vs 10586, P=0.016; Figure 2b. After treatment with HU both CD11b and CD18 expression decreased, though the differences did not reach statistical significance (P=0.22 and 0.56, respectively). Neutrophils of SCD patients displayed a more aged phenotype compared to neutrophils of HC with lower L-selectin (median MFI 3108 vs 4656, P=0.021) and higher CXCR4 (median MFI 1150 vs 886, P=0.003) expression. Activation marker CD64 was also higher in SCD patients compared to HC (median MFI 1841 vs 1065, P=0.0006). HU treatment seemed to modify all markers more towards a HC phenotype although no statistically significant changes were observed.
Conclusion Adhesion of both RBCs and neutrophils is increased in SCD patients compared to HC. HU treatment was associated with significantly improved RBC rheology as shown by decreased PoS and decreased adhesion to laminin. Despite a trend to improvement in expression of adhesion markers (CD11b/CD18), in vitro adhesion of neutrophils did not decrease. These findings could be due to the small sample size of patients starting with HU or by a difference in vitro behaviour of changed composition of neutrophil populations after treatment.
Disclosures
Biemond:GBT: Research Funding; BMS: Research Funding; BMS: Research Funding; Celgene: Membership on an entity's Board of Directors or advisory committees; Novo Nordisk: Membership on an entity's Board of Directors or advisory committees; CSL Behring: Membership on an entity's Board of Directors or advisory committees; Chiesi: Membership on an entity's Board of Directors or advisory committees; Bluebird Bio: Membership on an entity's Board of Directors or advisory committees; Bluebird Bio: Membership on an entity's Board of Directors or advisory committees; Modus Therapeutics: Membership on an entity's Board of Directors or advisory committees; Chiesi: Membership on an entity's Board of Directors or advisory committees; CSL Behring: Membership on an entity's Board of Directors or advisory committees; GBT: Membership on an entity's Board of Directors or advisory committees, Research Funding; Novo Nordisk: Membership on an entity's Board of Directors or advisory committees; Celgene: Membership on an entity's Board of Directors or advisory committees; Sanquin: Research Funding; Novartis: Membership on an entity's Board of Directors or advisory committees, Research Funding. Nur:Novartis: Membership on an entity's Board of Directors or advisory committees, Research Funding, Speakers Bureau.
Author notes
Asterisk with author names denotes non-ASH members.